Here we are going to share information on the topic “Signs of sickle cell disease in newborn babies.” The most prevalent inherited blood condition in the US is sickle cell disease. Children who have sickle cell disease have continuous medical difficulties as well as periods of excruciating anguish. Children with the disease can enjoy full and active lives and reduce their consequences with early and continued medical attention and therapy.

Signs of sickle cell disease in newborn babies
What effects does sickle cell illness have on kids?
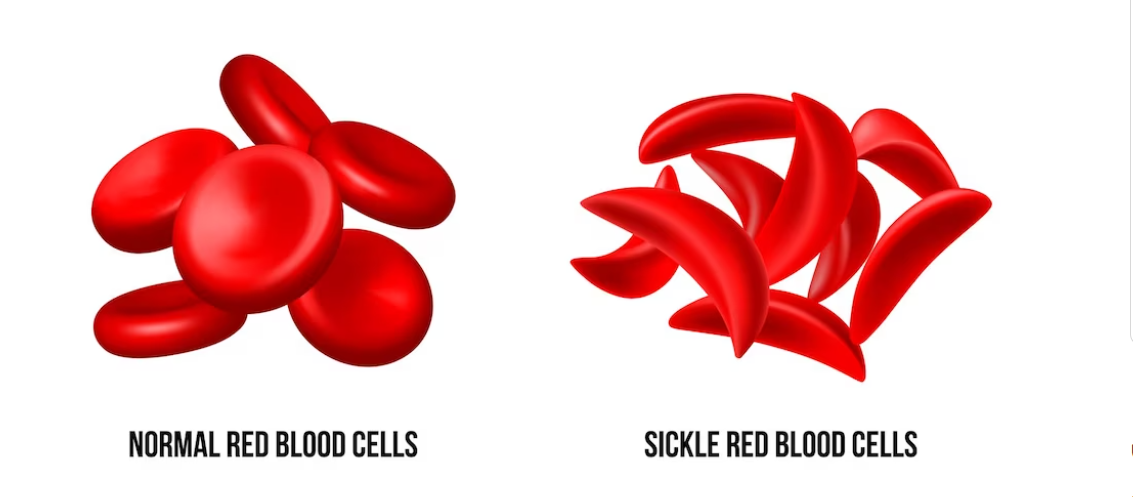
A protein called hemoglobin, which carries oxygen into red blood cells, clumps together in sickle cell disease-affected children’s red blood cells, giving them the appearance of a sickle cell, which is like a crescent moon or the letter C.
Sickled red blood cells are rigid, sticky, and brittle, in contrast to normal red blood cells, which have a disc shape and are flexible. Compared to regular red blood cells, they disintegrate and exit the bloodstream earlier. As a result, normal blood flow is blocked, which keeps blood and the oxygen it contains from reaching all parts of the body.
How does sickle cell disease affect young people?
A baby with sickle cell disease is born. Because sickle cell disease is a genetic disorder, children who have it inherit it in the same way that they get their skin, hair, and eye colors from their parents’ gene combinations.
How do people get sickle cell disease?
One hemoglobin gene came from their father and one from their mother. A characteristic is when a person inherits one aberrant or mutant gene from one parent while acquiring a normal gene from the other. The presence of sickle cell disease in a child is determined by the inheritance of two aberrant hemoglobin characteristics or genes.
The gene for normal haemoglobin is designated A. S or C denote the most prevalent mutant haemoglobin genes or haemoglobin characteristics. S is the haemoglobin gene that has been mutated or altered and is linked to sickle cell disease. S, C, and beta thalassemia are common forms of mutant (altered or aberrant) haemoglobin genes that combine with S to generate sickle cell disease.
Individuals with sickle cell disease are not those who have inherited any of the following gene combinations:
- A + A (AA): disease-free sickle cell
- A + S (AS): sickle cell trait carrier; carries the haemoglobin “S” gene.
- A + C (AC): the haemoglobin “C” gene carrier
Individuals with sickle cell disease do carry one of the following gene combinations in their genome:
- S + S (SS): Hemoglobin SS or sickle cell anemia
- S + C (SC): Hemoglobin SC or sickle haemoglobin C illness
- A type of sickle cell disease known as the S+ beta thalassemia trait, or S-beta thalassemia
What signs of sickle cell illness might a child have?
In their first year of life, most children with SCD will begin to exhibit symptoms, usually around the age of five months.
The symptoms in each child may differ. They could be minor or serious. Among the symptoms are:
Anemia
- The most typical symptom is this one. Anemia is the result of having fewer red blood cells. A youngster with anaemia may look pale and exhausted.
skin, eyes, and mouth yellowing (jaundice)
- This is a typical sign. Sickle cells have a shorter lifespan than healthy red blood cells. They pass away before the liver has time to remove them.
- When red blood cells die, a chemical called bilirubin is released, which is what gives the area its yellow hue.
A sickle crisis is a pain crisis.
- Sickle cells have the potential to become caught as they pass through tiny blood channels. Pain results from this blockage of blood flow.
- Though it can appear anywhere, the arms, legs, and chest are where it usually happens first. Painful swelling in the fingers and toes can occur in babies and early children.
- Tissue death may also result from obstructed blood flow.
symptoms of the acute chest.
- This occurs when sickle cells clump together and obstruct the lungs’ tiny blood capillaries’ ability to carry oxygen. This might be fatal.
- When the body is under stress from an infection, fever, or fluid loss, it frequently happens suddenly (dehydration). It can cause fever, pain, and a hacking cough, and it appears like pneumonia.
Sequestration of the spleen (pooling).
- When sickle cells become lodged and accumulate in the spleen, it enlarges and hurts. Red blood cells can travel less easily.
- Hemoglobin levels may suddenly plummet as a result. If treatment is delayed, it may be fatal.
Note: The signs and symptoms of SCD can mimic those of other illnesses or conditions.
Signs of sickle cell disease in newborn babies
How can I determine whether my child has sickle cell illness or trait?
In the United States, newborns are screened for sickle cell disease in every state. The infant is referred to a pediatric hematologist if the results of this test raise concerns about sickle cell disease. In most cases, a pediatrician will counsel the parents, and the child does not need to see a hematology specialist if the test results show sickle cell trait.
Infants with sickle cell disease can receive early treatment and a reduced risk of infections and other major issues if they are diagnosed before they exhibit any symptoms.
Why do children of African descent have a higher incidence of sickle cell disease?
The hemoglobin S trait, often known as the sickle cell trait, is the result of carrying a single haemoglobin S gene. S characteristic is present in about 1 in 12 people with African heritage. People having ancestors from the Caribbean, Middle East, India, South America, Central America, and Mediterranean nations like Greece, Italy, and Turkey also frequently have sickle cell trait. The sickle cell trait is now found in descendants of these groups, no matter where they live.
Sickle cell disease is not present in people who only have the haemoglobin S characteristic. However, they have a 1 in 4 (or 25%) chance of conceiving a child with sickle cell disease if their reproductive partner also carries the haemoglobin S trait. This explains why mixed and multiracial infants may be susceptible to sickle cell disease; in the US, approximately 1 in 365 black or African American babies are born with the disease each year.
Why is sickle cell anemia sometimes used to refer to sickle cell disease?
The general name for the various distinct forms of sickle cell illness is sickle cell disease. All kinds of sickle cell disease result in anemia, which is defined as a lower-than-normal haemoglobin level in red blood cells. Normal red blood cells can survive for 120 days, while sickled cells only last 7 to 20 days. Because the body cannot produce new sickled cells quickly enough, anemia results.
Sickle cell disease is a condition that affects children who have inherited two defective genes; the exact genes acquired determine the disorder’s name. Hemoglobin SS and sickle beta-zero thalassemia, the two most severe forms of sickle cell disease, are referred to as sickle cell anemia.
Hemoglobin SS is the primary kind of sickle cell disorder.
the most severe kind, which impacts 65% of kids with sickle cell disease. Chronic anaemia is brought on by aberrant haemoglobin, either in whole or in part.
Hemoglobin SC condition
This mild-to-severe variant of sickle cell disease affects about 25% of children with the illness. Though they may not always be as severe as in SS, symptoms usually appear later in childhood.
thalassemia + sickle beta
Around 8% of children with sickle cell illness are affected. Although severity can vary widely, this type of sickle cell disease is generally thought to be mild.
Beta-zero sickle cell thalassemia
a severe but uncommon variant that makes up 2% of cases of sickle cell illness. It is comparable to SS haemoglobin.
Why is the risk of infection higher in newborns and children with sickle cell disease?
- Brain, kidney, lung, and spleen damage are all possible side effects of sickle cell disease. The spleen may no longer be able to filter microorganisms from the blood as effectively as it once was due to sickled cells.
- Because of this, the immune systems of newborns and kids with sickle cell disease are weakened, making them more vulnerable to potentially lethal infections.
Antibiotics to stop children and newborns with sickle cell disease from getting secondary infections:
According to national standards, infants with severe sickle cell disease (SS and S beta-zero thalassemia) should be given antibiotics twice a day for five years.
According to research, children with sickle cell anemia who received penicillin twice a day had an 84 percent lower risk of contracting the bacterial infection Streptococcus pneumoniae, which can result in meningitis and pneumonia.
Is sickle cell illness curable or treatable?
Chronic illness is what sickle cell disease is. There were not many choices for treatment available until recently. Life expectancy has significantly increased in patients with severe forms of sickle cell disease when antibiotics are started shortly after delivery and diagnosis is made early.
Various alternatives are currently available based on the type of sickle cell condition to avoid major issues. These comprise hydroxyurea (for individuals 2 years of age and older), L-glutamine (5 years of age and above), voxeltor (4 years of age and above), and crizanlizumab (for individuals 16 years of age and older).
stem cell/bone marrow transplant. Sickle cell illness can be cured with this treatment. It is a process that uses bone marrow from a donor who has healthy cells to create blood. The bone marrow, which typically originates from a brother or sister, needs to match closely. For this approach, only about 25% of patients have a matched sibling who can donate.
gene treatments based on cells. New treatments (lovo-cel and exa-cel) for sickle cell disease have been approved by the Food and Drug Administration (FDA) for patients 12 years of age and older, particularly those who frequently experience severe symptoms from sickle cell that require hospitalization. The patients’ own blood stem cells are used in both treatments. They gather and alter their cells. After that, the patient is given a chemotherapeutic medication to extract bone marrow cells. Reconstituted stem cells are given back to the patients so they can create haemoglobin, which keeps red blood cells from clumping together. The National Human Genome Research Institute has additional information about gene therapy for sickle cell disease.
Signs of sickle cell disease in newborn babies
How is a child with sickle cell disease treated?
Your child’s age, overall health, and symptoms will all affect the course of treatment. Additionally, it will rely on how severe the situation is.
Treating this illness requires both early identification and preventing future issues. The doctor who treats your child will recommend a hematologist for you. This is a blood disorder expert. Your child’s care may also involve other professionals.
- Painkillers are among the possible treatments: Pain crises are addressed with these.
- Drinking a lot of water every day (8 to 10 glasses): Pain crises can be avoided and treated with this. IV (intravenous) fluids could be required in certain situations.
- Transfusions of blood: This is the procedure when your youngster receives donated blood via an arm vein. There is no blood taken from your child. It is used to prevent stroke and treat splenic sequestration, acute chest syndrome, chronic discomfort, and anemia.
- Interchange of red blood cells: At this point, a portion of the child’s red blood cells are extracted and replaced with donor-derived, healthy red blood cells. This may lessen the consequences of sickle cell disease.
- Both medications and vaccines serve as a defense against infections.
- folic acid: By doing this, severe anemia is avoided.
- Routine examinations of the eyes: These are done to check for retinopathy, an eye ailment. Every year, have your child’s eyes examined.
- Examinations using transcranial ultrasound: These are carried out to screen sickle cell patients who may be at risk of stroke.
- Transplant of stem cells: Some SCD patients can recover with transplants. Research on this therapy is still being done. Speak with your child’s medical professional. Only specific hospitals perform transplants.
- Hydroxyurea: This medication has the ability to lower the blood levels of sickle cells. It lowers the need for hospital stays, unpleasant episodes, and crises.
Research is still being done using the most recent medications. Talk about these options with your kids.
What are the potential side effects of pediatric sickle cell disease?
Among the SCD’s complications are:
- Chronic anemia: growth and development, as well as healing, may be postponed as a result.
- A sickle crisis is a pain crisis. In extreme circumstances, your child might require hospital care.
- Symptoms of the acute chest: Numerous acute chest syndrome events over time may result in long-term (permanent) lung damage.
- Sequestration of the spleen (pooling): The spleen swells up and hurts when red blood cells accumulate there. When splenic sequestration occurs repeatedly, the spleen may become injured and disfigured. Many eight-year-old SCD patients have had their spleen removed. Alternatively, the repeated splenic sequestration may have caused long-term harm. For kids without a functional spleen, infection risk is a big worry. For children under the age of five, infection is the leading cause of death.
- Stroke: A stroke may happen if the blood vessels that supply the brain are clogged. This could lead to severe long-term issues. A child’s risk of having another stroke is higher if they have already had one.
- Infections: Infants and kids with sickle cell disease are more susceptible to infections.
- Priapism: The blood vessels in the penis are blocked by sickle cells, resulting in a painful, protracted erection. If left untreated, this may result in the inability to achieve an erection (impotence).
Any main organ can be impacted by SCD. This may result in:
- recurring infections
- severe sores or leg ulcers
- bone injury
- Gallstones
- renal injury
- vision impairment
- failure of multiple organs
What support can I offer my child who has sickle cell disease?
Life-threatening sickle cell issues have decreased thanks to developments in preventive treatment and novel medications. However, the illness is still severe, persistent, and occasionally lethal. Professionals should be in charge of your child’s care. How you handle your child is determined by:
- Your child’s type of sickle cell
- The severity of the illness
- How frequently does your child experience difficulties?
- To what extent you and your child adhere to preventive measures?
It’s possible that you won’t be able to completely shield your child from SCD issues. However, you may lessen some of the issues by encouraging your child to lead a healthy lifestyle. Ensure that your child has screening tests for stroke and has regular eye exams.
Additionally, discuss with your child’s medical professional how to ensure that your child:
- consumes a balanced diet
- Obtains adequate rest
- consumes a lot of liquids
- Take caution when your youngster is exposed to specific things that could trigger a crisis. Among them are:
- elevated altitudes
- chilly conditions
- Taking a dip in frigid waters
Assist your kid in avoiding illnesses by:
- Remaining away from ill people
- frequently cleaning their hands
- With all recommended vaccinations, including influenza and pneumococcal
- Having undergone the recommended testing for hepatitis C,
- All sickle cell patients under the age of five receive penicillin on a regular basis to prevent infections.
That are the medical professionals who treat kids with sickle cell disease?
Children with sickle cell disease should see a pediatric hematologists on occasion in addition to seeing their pediatrician on a regular basis. These medical professionals are experts in treating young patients with sickle cell disease.
Conclusion
Signs of sickle cell disease in newborn babies
In summary, early diagnosis and treatments for sickle cell disease in newborns depend on identifying the symptoms. Being on the lookout for symptoms like pallor, jaundice, and trouble breathing might be crucial in securing prompt medical attention. Effective management and treatment of this hereditary disorder require regular newborn screenings, genetic counselling, and increased awareness among parents and medical providers. Early identification raises the chances of a successful course of therapy and favorable long-term health outcomes, in addition to improving the quality of life for impacted newborns.

Frequently asked questions
Signs of sickle cell disease in newborn babies
Can a child with sickle cell live a normal life?
Answer: Sickle cell illness patients are capable of leading full, active lives.
By visiting their physician on a regular basis and following preventative measures, such as frequent hand washing, people with sickle cell disease (SCD) can reduce their risk of experiencing complications from the disease and continue to engage in many normal activities.
What is the age limit for sickle cell?
Answer: Although the life expectancy of SCD patients has increased due to new treatments and optimal disease management, with patients now living past the age of 50, the life expectancy of SCD patients is still approximately 20 years shorter than that of the general population, and the quality of life is frequently poor.
How do I know if my baby has sickle cell?
Answer: How Is the Diagnosis of Sickle Cell Disease Made? During standard newborn screening examinations, sickle cell illness and sickle cell trait are typically detected at birth by blood testing. The diagnosis will be verified by a haemoglobin electrophoresis, a second blood test.
What should kids with sickle cell avoid?
Answer: Take precautions to avoid getting sick.
Salmonella infections are more common in children with sickle cell disorder. Bacteria include the type Salmonella. Your youngster should not eat raw or undercooked meats or eggs to avoid contracting salmonella. Verify the status of your child’s vaccinations.
At what age does sickle cell pain start?
Answer: Individuals who have sickle cell disease (SCD) typically exhibit symptoms for the first year of life, beginning at age five months. Each person experiences SCD symptoms and complications differently, and they can range in severity from moderate to severe.
Which organ is most affected in sickle cell Anemia?
Answer: The spleen aids in removing infections from the circulation. Dead cells are trapped in this filter and eventually perish. Chronic anaemia can occur when the body produces fewer healthy red blood cells. The spleen is also harmed by the sickled cells.