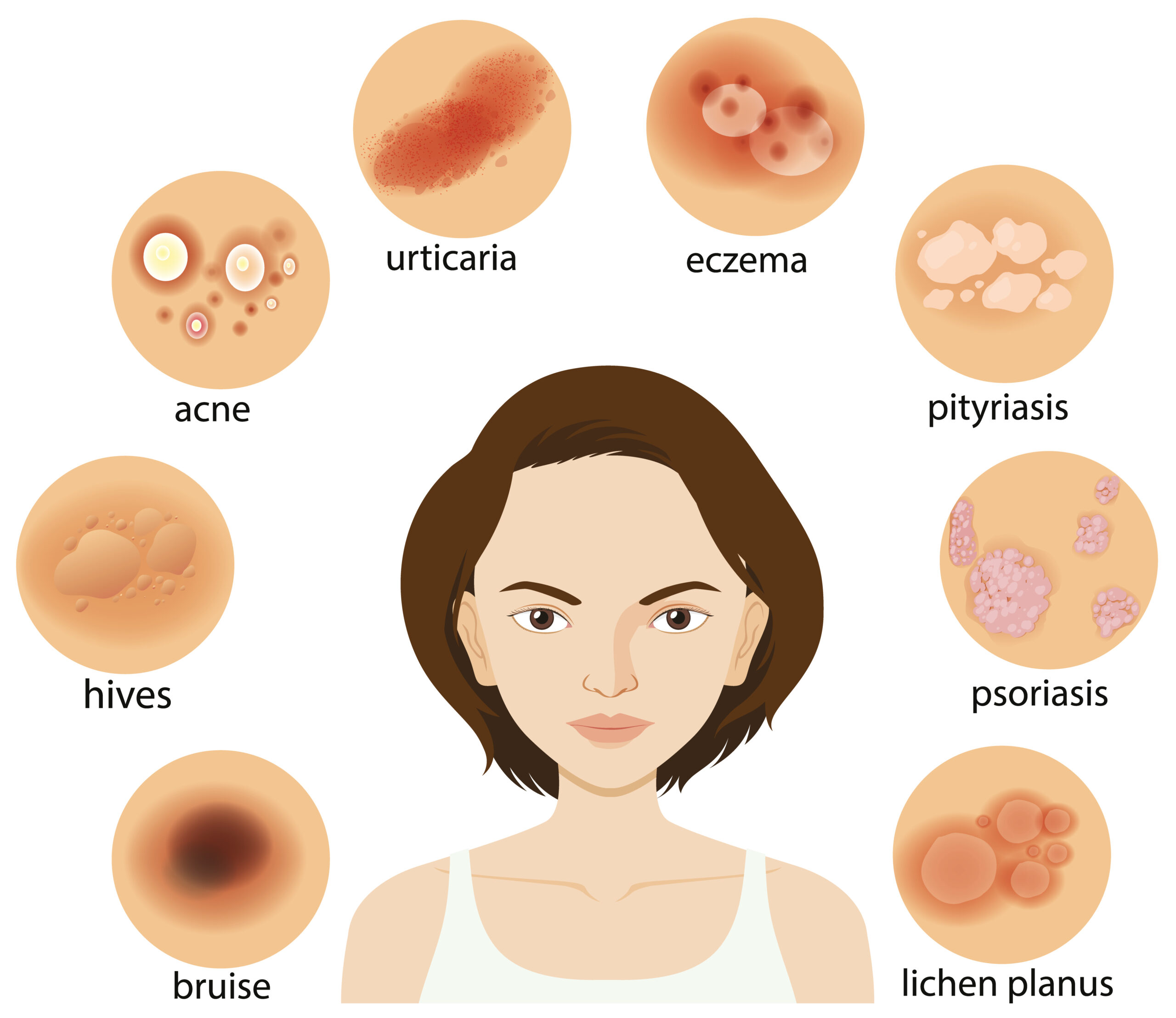
Here we are going to share information on the topic “20 Types of Skin Lesions.” Unusual alterations in the skin in relation to the surrounding tissue are called skin lesions. Skin lesions can have a smooth appearance or resemble lumps or spots. They could have a distinct texture or color from the skin around them.
Acne, cellulitis, and chickenpox are common reasons. This article examines 20 different kinds of skin lesions, along with their causes, images, and methods of care.

20 Types of Skin Lesions
Skin Lesions: What Are They?
Any spot of skin that differs from the surrounding skin is referred to as a “skin lesion.”
Skin lesions might be flat, like an age spot, or elevated, like a cyst. They may resemble a melanoma that is asymmetrical or a wart that is symmetrical. Certain lesions, like skin tags, match your skin tone perfectly, while other lesions, like moles, are darker.
There are a wide variety of skin lesions that you can either develop or inherit from birth. Certain things are innocuous, meaning they don’t hurt others. Some may be malignant and extremely severe. They could show up in one area of your body or all over it like hives.
Identification of a skin lesion might be aided by its appearance and location. When diagnosing a skin lesion, medical professionals take into account:
- Color
- Size
- Texture
- Location
20 Types of Skin Lesions
Skin Lesion Types
1. Acne
The main symptom of acne is papules. Moreover, it may result in cysts, nodules, or pustules. The following locations have the highest rates of acne:
- Face
- Neck
- Chest
- Back
If acne is not treated, scars may result.
When sebum, an oily discharge, or dead skin cells clog your pores, acne results. An overabundance of a particular type of bacteria on the skin may potentially be the cause.
2. Keratosis Actinic
Sun exposure is the cause of actinic keratosis. On the skin, it manifests as thick, scaly crusts. The majority of those over 40 have it. Typically, it takes longer to manifest in later life due to its association with years of sun exposure.
Its surface is elevated and covered in scales. This makes feeling, rather than seeing, easier. It may become hard and wart-like over time. It might acquire a texture akin to a horn.
3. Blisters
The skin’s liquid-filled spots are called blisters. Friction from your shoes rubbing against your skin while you walk may be the source of them. They may also result from an allergic response, a skin condition, or a burn.
Blisters may usually be taken care of at home. Don’t pop blisters, please. Refrain from applying extra pressure to the blistered region.
Cleanse the area if a blister does burst. Till it heals, wrap it with a sterile bandage.
Consult a physician if you exhibit any of the following infection symptoms:
- Pus, a viscous greenish-yellow discharge
- Fever
- heated, red skin surrounding the blister
A blister is referred to as a vesicle if it is smaller than 0.5 cm. It is referred to be a bulla when it is larger than 0.5 cm.
4. Cellulitis
A skin infection is called cellulitis. It takes place when fungi or bacteria get under the skin.
Cellulitis symptoms include:
- Pain Pain Swelling Redness
- Fluid seeping out
- To the touch, cellulitis feels heated.
- You can feel sick and develop a fever as a result of it.
Most instances can be treated at home with antibiotics if they are discovered early. Severe and dangerous problems may arise if treatment is not received. Hospitalization may be required on occasion.
When to Get Medical Help
Seeing a physician is crucial if you exhibit any cellulitis symptoms. Seek immediate medical attention if you observe any parts of your skin that are swollen, red, painful, or heated, especially if you have recently sustained a cut, bite, or burn.
5. Chickenpox
Varicella, another name for chickenpox, is a viral skin ailment.
Red, fluid-filled blisters cover the entire body when a person has chickenpox. Usually, they cause itchiness and heat. Pus may seep from the blisters and result in subsequent crusting.
A person can contract chickenpox two days prior to the rash developing. Until all of the blisters have crusted over, it is still communicable.
At-home detection of chickenpox is feasible. To get the diagnosis confirmed, you might choose to visit a medical professional.
6. Comedones
Acne can take the form of comedones.
There are several varieties available:
Open comedones, or blackheads, indicate that the pore is still open. There is a dark area in the centre of them.
Smooth, painless, and soft, closed comedones.
White heads are seen on hard-closed comedones. Another name for them is Milia. They are not to be confused with pus-filled whiteheads.
7. Cold Sores
Sores on the lips or mouth are known as cold sores. The herpes simplex virus (HSV) is the source of them.
Cold sores can create blisters packed with fluid, appear red, and hurt. Tinting could occur prior to the sore showing up. As a result of the virus that causes them, you can also experience flu-like symptoms.
Treatment from a healthcare professional may be necessary for really acute cold sores or sores that don’t seem to be healing on their own.
HSV-2 versus HSV-1
Dissimilarities exist between HSV-1 and HSV-2
Oral herpes is typically caused by HSV-1. The mouth and lip regions become infected with fever blisters and cold sores.
The typical cause of genital herpes is HSV-2.
Either virus, though, has the potential to produce genital or oral outbreaks.
Get in touch with dermatitis
A material that irritates the skin or an allergen is the cause of contact dermatitis.
Symptoms often only show up where the irritant comes into contact with the skin.
Among the symptoms could be:
- Redness
- Itching
- Macules
- Papules
- Fissures
- Blisters
- Plaques
- Increased Sensitivity to Touch
- Chafing
Consult a physician if your contact dermatitis does not improve at home.
8. Eczema
Another name for eczema is atopic dermatitis. It manifests as a red, itchy rash.
Among the symptoms could be:
- Yellow, brown, grey, or red skin patches
- Itching
- Dryness
- Blisters
- Fissures
- Plaques
- uncomfortable and sensitive areas
The weather, whether it be hot or cold, might trigger a flare-up of symptoms. Additionally, some skin care products could irritate your skin. It is common for food allergies, hormone fluctuations, and dust mites to exacerbate symptoms.
The most popular forms of treatment consist of:
- Using an emollient, such as a moisturizer, to keep skin hydrated
- creams and soaps for the skin
- cream containing corticosteroids
- Steer clear of irritants and triggers
Over-the-counter medications can be used at home to treat mild eczema. Your dermatologist or primary care physician can assist you in creating a treatment plan if your eczema is more severe.
9. Freckles
On the skin, freckles are tiny, flat, light-brown macules. The sun is the cause of them.
Freckles are generally benign and infrequently develop into skin cancer. Those with red hair or light, fair skin tend to have them more frequently.
Treatment for freckles is rarely necessary unless they alter or there is a suspicion of skin malignancy.
Sun Lentigines and Ephelides
Common names for these two kinds of lesions are freckles:
Ephelides:
Common freckles that have appeared since childhood are these:. Those with red hair and/or fair skin seem to have them more frequently. They are typically millimetres in size and spherical in shape. They come in different tones of brown.
Sun lentigines
Solar lentigines are distinct-bordered macules. They range from pale brown to dark brown. The most common names for them are actinic lentigines, sun spots, liver spots, and ageing spots. They are most frequently observed in older people and are brought on by prolonged sun exposure.
10. Hives
Another name for hives is urticaria. They resemble elevated, red, puffy spots on the skin.
Usually, an allergic reaction to a particular substance results in hives. They may also occur for unidentified causes.
Hives may hurt or be itchy. The individual marks usually disappear after less than a day, although additional marks may still show up.
11. Impetigo
A bacterial skin infection called impetigo. It is brought on by germs getting into the skin via a tiny cut or hair follicle. The ailment results in blister-like lumps, crusts, and sores.
Impetigo spreads easily. Typically, it impacts young toddlers the most.
12. Keloids
After an accident, keloids are elevated scars that develop. Their hues vary from red to flesh-colored. The excessive growth of scar tissue that results in keloids frequently causes discomfort and itching.
Certain individuals have a higher risk of acquiring keloids. On the other hand, several preventive steps might prevent keloids from developing.
- Individuals who have previously experienced keloids are more likely to experience them again. There are a couple things you can do to stop this:
- Injured regions should be closely monitored for any thickening of the skin. For example, if you discover this after getting your ear pierced, take out the earring right away and cover the piercing with a pressure earring.
- Take good care of your wounds. Use sterile petroleum gauze to bandage after washing with soap and water. On recently healed scars, apply silicone sheets or silicone gel.
- Keloids don’t need to be treated medically because they are safe. Nonetheless, some people’s self-esteem may be damaged by their appearance. See your dermatologist if you observe any thickening of the skin surrounding a wound that has just healed. Their appearance might be lessened with treatment.
13. Moles
A mole may also be referred to as a nevus or melanocytic nevus. Usually, they are nodules, papules, or circular, brown or pink macules. They can develop at any age and can be located anywhere on the body.
Generally speaking, moles are benign. But if a mole changes in size, colour, or shape, or starts to bleed or crust, you should consult a physician. This may indicate melanoma, a form of skin cancer.
ABCDE Guideline
These alterations, when observed in your moles, may indicate melanoma:
- Asymmetrical: Take a look at the mole’s form. Moles often have a uniform shape and appearance from all angles. Melanomas frequently have irregular shapes.
- Normal moles have a smooth border around them. Usually, melanomas have a jagged, uneven border.
- Moles typically have a uniform hue throughout. Melanomas may have varying colours.
- In general, moles have a tiny diameter. Most melanomas have a width of more than 6 millimetres.
- Evolving: Not much changes in moles over time. Melanomas frequently alter in texture, colour, size, or shape.
Watch for any changes in your moles or for any new moles that exhibit these characteristics. See a healthcare professional as soon as possible if you discover anything odd.
14. Psoriasis
Fair-skinned individuals with psoriasis typically have red, flaky skin, crusty skin patches, and silvery skin scales. Silvery-white scales and salmon-colored psoriasis are more common in Hispanics. Psoriasis frequently appears violet and has gray scales in African Americans.
The body creates skin cells too quickly—over the course of days as opposed to weeks—which leads to psoriasis. Patches that are thick, elevated, and scaly result from excessive skin cell proliferation.
The following are the places where psoriasis is most common:
- Knees
- Elbows
- Scalp
- back of the lower back
Nevertheless, it can happen elsewhere on the body. Psoriasis does not have a treatment.
15. Scabies
A mite is the cause of scabies. The itching is severe at first. There may also be a rash. Small red papules, welts, or scaly lesions can be the appearance of the rash. Scratching repeatedly might harm the epidermis.
16. Sebaceous Cyst
Round, keratin-filled sebaceous cysts are loaded with the same protein that makes up skin, hair, and nails. The nodules are often skin-colored and hard. Usually, they show up on the face or upper torso. They can vary in size and sometimes burst.
It is necessary to treat a ruptured cyst in case it becomes infectious. Other than that, sebaceous cysts typically don’t need to be treated. They are generally benign and grow slowly.
17. Shingles
The virus that causes chickenpox reactivates to produce shingles. A rash with blisters, papules, and macules that is red and extremely painful is called shingles. The blisters may rupture and release liquid. There may be secondary crusting as a result.
The rash might hurt and itches and burns. Additional signs and symptoms may consist of:
- Fever
- Chills
- Headache
- Lethargy
Shingles can also be referred to as bands or belt. This is due to the fact that it frequently resembles a belt around the waist or rib cage.
Vaccines such as Shingrix can lower the chance of developing shingles. The Shingrix vaccine is advised by the Centers for Disease Control and Prevention (CDC) for persons over 50 and younger adults with compromised immune systems. Additionally, the vaccine guards against postherpetic neuralgia, a painful nerve disorder. This is the most typical shingles-related problem.
18. Skin Tag
Another name for skin tags is acrochordon. These are tiny, skin-colored growths that are soft and increasingly common as people age.
- In most cases, removal is not required. Usually, skin tags don’t need to be treated medically unless:
- They give rise to concerns regarding appearance.
- They’re in an uncomfortable position.
Human papillomavirus (HPV) is the cause of warts. They are infectious and frequently occur in groups.
19. Warts
Warts are flesh-colored, elevated papules. There could be little black spots in the middle of them. Although they are not harmful, they can cause pain and are easily contagious.
There are numerous varieties of warts, such as:
- Typical warts
- plantar warts
- Warts that are flat
- Warts that are filiform
- Warts on the genitalia
- Warts periungual
Most warts don’t pose a threat. Cervical or anal cancer is an uncommon side effect of several human papillomavirus types that cause genital warts.
Skin lesions are either primary or secondary. Primary skin lesions are either present from birth or develop during your lifetime.
20. Principal lesions on the skin
Generally speaking, primary skin lesions fall into three categories:
Lesions resulting from fluid accumulation in the skin layers: vesicles and pustules are two examples.
Solid mass lesions—tumors and nodules—are two examples.
Patches and macules are two types of flat lesions.
How Are Skin Illnesses Identified?
Make an appointment to get a lesion examined by a dermatologist or healthcare provider as soon as you find one on your skin. They will physically inspect the lesion during your visit, taking note of its size, shape, colour, texture, and location.
Your healthcare professional will inquire about the lesion, including when you first noticed the skin change and whether it itches. They will also likely ask you about any allergies or medical disorders you may have, any drugs you take, and other details related to your past health.
- Medical professionals can frequently identify skin lesions only by observing them. Nevertheless, in order to confirm a diagnosis, they could request other testing, such as:
- An allergy test to determine whether a person is hypersensitive to a particular allergen, such as a skin prick test
- A blood test to look for immune system activity that can indicate an infection or skin disease, such as an immunoglobulin E (IgE) blood test
- A microbiological swab is used to identify any bacteria or fungi that may be responsible for the lesion
- A skin biopsy to identify cancer or rule it out (cancer)
How Are Skin Irritations Handled?
The majority of skin lesions are benign (harmless) and don’t require removal unless they are for aesthetic purposes. If the lesion is bothering you or if there is any concern that it could be cancerous, your doctor might advise having it removed.
The majority of the time, skin lesions can be removed at the doctor’s office, but occasionally a surgeon may be required. Prior to removal, a local anaesthetic will probably be used to numb the lesion and the surrounding skin.
Frequently asked questions
20 Types of Skin Lesions
What are the 3 types of skin lesions?
Primary lesions are skin abnormalities that don’t correspond with other medical disorders. These include:
a level spot on your body that is not the same colour as your skin tone (macule or patch).
A raised protrusion like a pimple (papule or plaque).
A solid, raised bump (nodule).
What is the skin lesion classification?
The lesion must be identified as melanoma (Mel), nevus (Nev), or seborrheic keratosis (SK) in the ISIC-Mel. Nevus (Nev), Seborrheic Keratosis (SK), Basal Cell Carcinoma (BCC), Actinic Keratosis (AK), Dermatofibroma (DF), Vascular Lesion (VL), and Melanoma are the seven classifications that make up the ISIC (Mel).
What is the category of skin lesions?
There are two types of skin lesions: primary and secondary. Primary skin lesions are aberrant skin conditions that may exist from birth or develop over time. Exacerbation or modification of initial skin lesions might result in the development of secondary skin lesions.
What is the classification of lesions?
Skin lesions can be categorised by doctors into many types, including pigmented benign keratosis (BKL), basal cell carcinoma (BCC), squamous cell carcinoma, benign or non-malignant nevus, and dangerous melanoma (SCC).
What is ABCD in skin lesions?
When applied retrospectively to clinical slides, the recently developed ABCD rule of dermatoscopy (skin surface microscopy at x10 magnification) enhanced diagnostic accuracy. It is based on the criteria of asymmetry (A), border (B), colour (C), and differential structure (D).
What is a basic skin lesion?
Primary and secondary skin lesions are the two main categories into which they fall. Primary skin lesions have a clear aetiology and begin on skin that was previously healthy. Primary skin lesions are frequently seen as blisters, moles, and freckles, among other things.

Conclusion
20 Types of Skin Lesions
These lesions can arise from various causes, including infections, inflammatory conditions, allergic reactions, autoimmune disorders, trauma, and malignancies. Proper diagnosis and treatment depend on identifying the underlying cause and type of skin lesion.
So, this is how the topic “20 Types of Skin Lesions” has been addressed.
For more information related to these topics,
You may also visit our Instagram page by
Thank you!