Here we are going to share information on the topic “peripheral artery disease symptoms.” Plaque, which is a buildup of lipids and cholesterol in the arteries in your arms and legs, is known as peripheral arterial disease, or PAD. Your blood has a harder time getting oxygen and nutrients to the tissues in certain places as a result. Although PAD is a chronic condition, you can live a better life by exercising, cutting back on fat, and quitting smoking.

peripheral artery disease symptoms
Peripheral arterial disease: what is it?
Plaque accumulation in the arteries in your legs is known as peripheral arterial disease, or PAD. Your leg arteries provide your arms and legs with blood that is rich in nutrients and oxygen from your heart. Peripheral vascular disease and peripheral arterial disease are other terms for this.
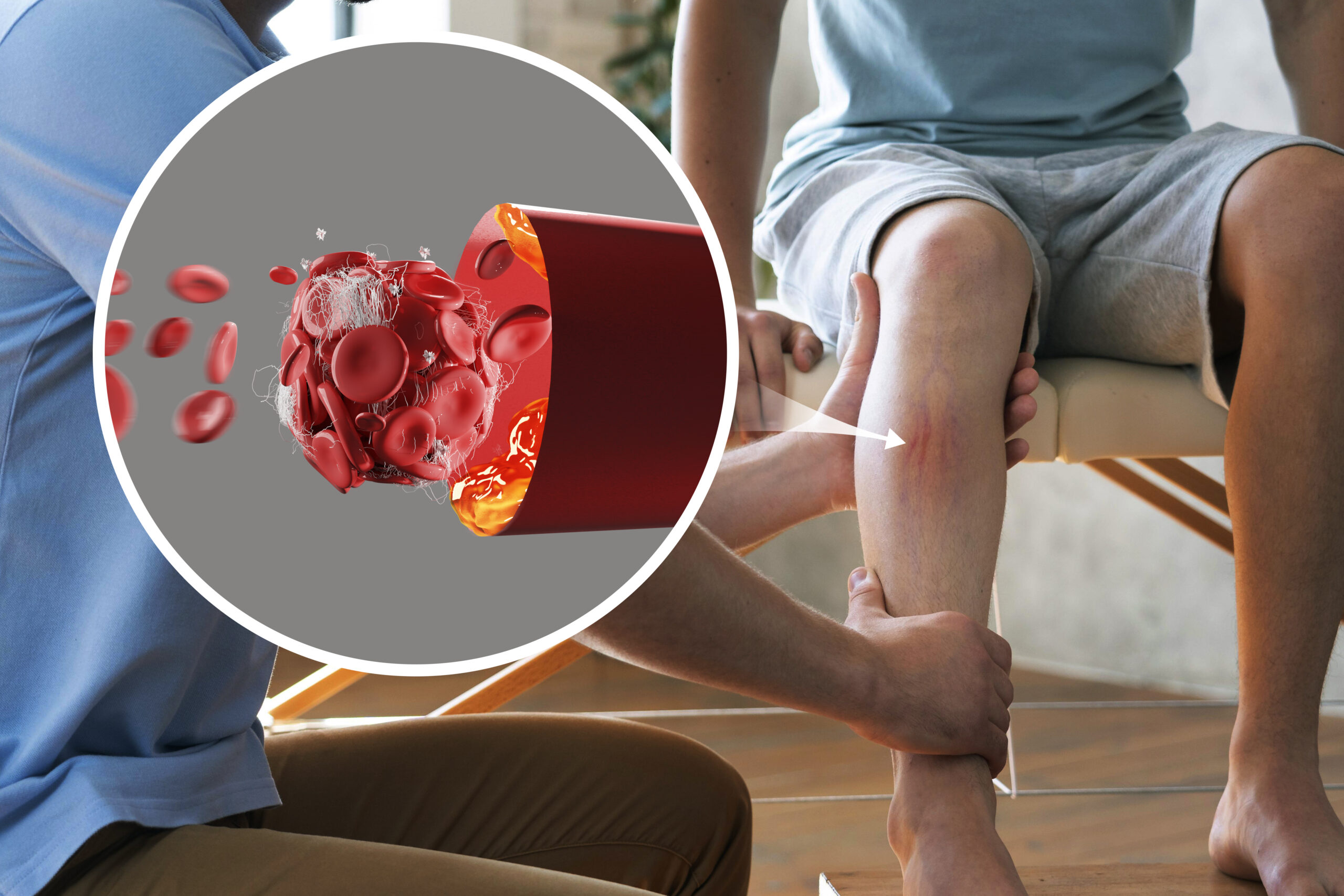
Arteries resemble hollow tubes and are lined with a smooth substance that keeps blood from clotting and encourages constant blood flow. Plaque, which is composed of fat, cholesterol, and other materials, progressively accumulates inside the artery walls of people with peripheral artery disease. This narrows your arteries gradually. Another name for this plaque is atherosclerosis.
A lot of plaque deposits have a soft interior and a hard exterior. The hard surface may break or tear, allowing platelets—which are blood clotting particles in the shape of discs—to enter the area. The plaque may cause blood clots to form, narrowing your artery even more.
Blood cannot flow through narrowed or blocked arteries to supply organs and other tissues. This is caused by plaque or blood clots. This harms the tissues beneath the obstruction, leading to eventual death (gangrene). Your feet and toes are where this most frequently occurs.
For some people, PAD can worsen more quickly than for others. Numerous other criteria are important as well, such as the location of the plaque in your body and your general health.
Is peripheral artery disease common?
In America, PAD affects 8 to 12 million people on a regular basis. But occasionally, medical professionals fail to adequately diagnose or treat PAD. The real figures are most likely greater.
What physical effects does peripheral artery disease cause?
Claudication, a medical term for leg pain that begins with walking or exercise and subsides with rest, is the most common symptom of PAD. Your leg muscles aren’t getting enough oxygen, which is the cause of the pain.
The risks associated with PAD go far beyond walking limitations. Your legs or feet can become infected with a non-healing sore if you have peripheral artery disease. These lesions may develop into gangrenous areas in situations of severe PAD, necessitating the amputation of your foot or leg.
What stages does peripheral artery disease go through?
To assign a stage to your PAD, medical professionals might use the Fontaine and Rutherford methods. The easier Fontaine stages are as follows:
I: Lack of symptoms (without symptoms).
II: mild dysphagia (leg pain during exercise).
II: Severe to moderate
III: Ischemic rest pain, which is pain in the lower limbs during repose.
IV: Gangrene or ulcers.
Signs and Origins
What is thought to be peripheral artery disease’s initial symptom?
Usually, pain, cramping, or discomfort in the legs or buttocks is the initial sign of PAD (intermittent claudication). This occurs during physical activity and disappears during sleep.
What signs and symptoms of peripheral artery disease are common?
Peripheral artery disease symptoms include:
- A pain in your feet and toes that burns or aches when you’re sleeping, especially at night when you’re flat on your back,.
- Your feet’s cool skin.
- redness or other variations in skin tone.
- increased occurrence of soft tissue and skin infections (usually in your feet or legs).
- Foot and toe sores that refuse to go away.
Peripheral vascular disease affects 50% of patients without any symptoms. PAD can accumulate over a person’s life. It’s possible for symptoms to hide until later in life. Many individuals won’t experience symptoms until their artery narrows by 60% or more.
If you suspect you may have PAD, consult a healthcare professional so that treatment can begin right away. It’s critical to discover PAD early in order to start the appropriate treatments before the condition worsens to the point where consequences like a heart attack or stroke occur.
What side effects might peripheral artery disease cause?
If therapy is not received, individuals with PAD may require an amputation, which involves amputating all or a portion of the foot, leg, or arm (rarely the arm), particularly if they also have diabetes.
The symptoms of peripheral artery disease (PAD) can go beyond the limb that is damaged since your body’s circulatory system is linked. Individuals who have leg atherosclerosis frequently also have it in other body areas.
What causes peripheral artery disease the most frequently?
Peripheral arterial disease is caused by atherosclerosis that occurs in the arteries of the arms or legs; however, it is less common in the former case. Peripheral vascular disease is caused by a buildup of fatty plaque in the blood vessel walls, similar to atherosclerosis in the coronary (heart) arteries. Your blood vessels become narrower and narrower until they become clogged when plaque accumulates.
What are the peripheral artery disease risk factors?
The primary risk factor for PAD and its consequences is tobacco smoking. As a matter of fact, eighty percent of those diagnosed with PAD are smokers or former smokers. The risk of PAD increases by 400% with tobacco usage. Additionally, it triggers PAD symptoms nearly ten years earlier.
People with PAD who smoke have higher odds of the following as compared to nonsmokers of the same age:
- Die from a stroke or heart attack.
- Have less favourable outcomes from leg bypass surgery treatments.
- Get a limb amputated.
If you have one or more of the following risk factors, peripheral arterial disease is a possibility for you, regardless of your gender:
Using tobacco products (the most potent risk factor).
- being diabetic.
- being fifty years of age or older.
- being of African American descent.
- has a family or personal history of blood vessel or heart illness.
- Experiencing elevated blood pressure (hypertension).
- Having elevated cholesterol levels (hyperlipidemia).
- being obese in the abdomen.
- having a problem with blood coagulation.
- suffering from renal illness (both a risk factor and a consequence of PAD).
Despite being distinct conditions, coronary artery disease and peripheral artery disease are connected. Individuals with one are more likely to have the other. Compared to someone without peripheral arterial disease, a person with PAD is more likely to experience a heart attack, stroke, coronary artery disease, or transient ischemic attack (mini-stroke). Peripheral artery disease in the legs is one in three times more likely to strike a person with heart disease.
Unsurprisingly, there are some risk factors in common between the two diseases as well. This is due to the fact that these risk factors alter the arteries in your arms and legs in the same way that they alter the arteries in your heart.
Diagnoses and Examinations
How can one diagnose peripheral artery disease?
Along with reviewing your medical history and risk factors, the provider will do a physical examination. To help diagnose and assess the severity of PAD, they could prescribe noninvasive tests. These tests can assist in identifying any blood vessel blockages you may have.
- Brachial-ankle index (ABI).
- recording of pulse volume (PVR).
- ultrasonography of the arteries.
- To identify arterial blockages, you could also require an invasive test called an angiography.
Handling and Medical Interventions
Is it possible to reverse peripheral artery disease?
Yes. Exercise, along with controlling blood pressure and cholesterol, has been demonstrated in certain trials to be able to reverse the symptoms of peripheral vascular disease.
You can prevent PAD from getting worse with early diagnosis, therapy, and lifestyle modifications. Speak with your health care physician, vascular medicine specialist, or cardiologist if you believe you may already have PAD or are at risk for the condition. This will enable you to begin a preventative or treatment programme right away.
How does one treat peripheral arterial disease?
- PAD can be treated with operations, drugs, and changes in lifestyle.
- Reducing the risk of cardiovascular events is one of the two main objectives of treatment for peripheral artery disease.
- reducing the discomfort that comes with walking and enhancing your quality of life.
Modifications in lifestyle
The first step in treating PAD is changing your lifestyle to lower your risk factors. Among the adjustments you can make to control your condition are:
- Give up using tobacco products. Find out more about smoking cessation programmes from your healthcare professional.
- Consume a well-balanced diet that is low in fat, cholesterol, and sodium and high in fibre. Limit your fat intake to
- 30% of your daily caloric intake. You should consume no more than 7% of your calories from saturated fat. Steer clear of trans fats, including those found in goods containing hydrogenated and partially hydrogenated vegetable oils.
- Exercise. Begin a regular fitness regimen, like walking. PAD can be treated with walking. Regular walkers are able to extend the distance they can cover before experiencing leg pain.
- Handle additional medical issues, including diabetes, high blood pressure, or high cholesterol.
- Maintain a modest level of tension. Yoga, meditation, and exercise could be helpful here.
- To lower the risk of problems and avoid infection, take appropriate care of your skin and feet.
Medications
Conditions, including diabetes, high blood pressure, high cholesterol, and antihypertensive drugs, can all be treated with medicine. These medications lower your risk of heart attack and stroke while treating PAD risk factors.
Aspirin and clopidogrel are two examples of antiplatelet medications that your doctor may prescribe. Additionally, they might recommend Cilostazol to increase your walking distance. This drug helps patients with intermittent claudication exercise more frequently before experiencing leg pain.
Exercise regimens under supervision
Walking pain in your legs can be reduced with a supervised fitness programme, enabling you to go farther. A structured programme usually consists of at least three times a week of supervised treadmill walking.
It is recommended that individuals with PAD walk for a minimum of 30 to 60 minutes each day while at home. The “Start/Stop” exercise is the standard prescription:
- Stroll until you feel a modest amount of discomfort, and then stop.
- Hold off until all the soreness has subsided.
- Go back to walking.
- therapies that are surgical or minimally invasive
Even after a few months of exercise and medication, leg discomfort may remain a daily concern for some people with more severe PAD. In more extreme situations, patients require improved blood flow to heal a wound or reduce discomfort while at rest.
Treatment options for more advanced PAD that’s limiting movement and producing excruciating pain could include surgery or endovascular (minimally invasive) procedures. Peripheral artery disease is treated with certain heart disease medications, such as:
- Angioplasty.
- Stents.
- surgery to bypass peripheral arteries.
- Atherectomy.
- Treatment complications for PADs
If these problems persist after your operation, you should speak with your healthcare provider. These can indicate an infection or other problems.
- soreness, bleeding, or swelling where the skin was punctured by the catheter.
- ache in the chest.
- breathlessness.
- chills or fever.
- Dizziness.
- enlargement of the legs.
- stomach ache.
- A wound that is opening up.
How long does it take to recover from treatment for peripheral artery disease?
You could stay in the hospital for one or more nights, depending on the therapy you received. An atherectomy may just require a few days to heal. However, a week will pass following an angioplasty. Complete recovery from peripheral artery bypass surgery might take up to eight weeks.
Prevention
How may peripheral artery disease be prevented?
Being aware of your PAD risk factors could inspire you to avoid them. The following guidelines also apply to maintaining the health of your circulation:
- Control your weight.
- Consume at least five servings of fresh fruits and vegetables each day as part of a low-fat, low-sugar diet.
- Use no tobacco products at all.
- Exercise for at least 30 minutes a day, most days of the week, with your doctor’s consent.
Talk to your healthcare physician about your PAD risk factors if you have heart disease. Report any symptoms you’re experiencing, including any leg pain, weakness, or numbness.
Prognosis and Outlook
If I have peripheral artery disease, what can I anticipate?
Similar to most medical diseases, PAD is easier to treat the earlier a practitioner detects it. Different people develop peripheral vascular disease at different rates. This is dependent on a number of variables, such as your general health and the location of the plaque in your body.
Prognosis for peripheral arterial disease
You will have peripheral artery disease for the remainder of your life. PAD cannot be cured, but it is manageable. There are multiple ways in which you can prevent the progression of peripheral vascular disease:
- abstaining from tobacco products.
- engaging in regular exercise.
- consuming less fat and maintaining a balanced diet.
- Controlling your risk factors, which include high blood pressure, high cholesterol, and diabetes,.
How do I look after my needs?
Maintaining proper foot care is essential to avoiding non-healing blisters. For those with PAD, foot care involves:
- wearing shoes that fit well and are comfortable.
- checking your feet and legs every day for sores, cuts, cracks, blisters, and scrapes. Additionally, look for calluses, corns, ingrown toenails, redness, and increased temperature.
- Not putting off taking care of a small skin or foot issue.
- Keeping your feet moisturised and clean. (An area with an open sore shouldn’t be moisturised.)
- After taking a bath, trim your toenails while they’re still tender. Use a nail file to smooth them after making a straight cut across them.
When it comes to specialist foot care, particularly if you have diabetes, your healthcare practitioner might occasionally recommend that you see a podiatrist, or “foot expert.” If you have corns, calluses, or other foot issues, a podiatrist can assist you.
When should I visit my medical professional?
Speak with your physician if you:
Get a serious infection in your foot. The infection has the potential to spread to your bones, blood, muscles, and tissues. Should your infection be serious, a hospital visit might be necessary.
unable to move about sufficiently to perform daily tasks.
Experiencing discomfort in your legs while at rest. This indicates inadequate blood flow.
Frequently asked questions
peripheral artery disease symptoms
Symptoms
- feeling of coldness in the foot or lower leg, particularly in relation to the opposite side.
- legs feeling weak or numb.
- The legs or feet may not pulse at all or rather weakly.
- cramping that hurts in one or both hip, thigh, or calf muscles during strenuous activity like walking or climbing stairs.
- The legs’ skin is shiny.
Which is the most common location for peripheral artery disease?
Although PAD can occur in any blood vessel, it tends to occur more frequently in the legs than the arms.
Is peripheral artery disease serious?
Although PAD does not immediately pose a threat to life, the atherosclerotic process that produces it can result in significant and even deadly issues.
Can PAD disease be cured?
Contents. Peripheral arterial disease (PAD) has no known cure; however, medication and lifestyle modifications might lessen symptoms. Additionally, these therapies may lessen your chance of contracting coronary heart disease and other forms of cardiovascular disease (CVD).
How can I test for peripheral artery disease at home?
Test of Leg Elevation
On a bed, lie on your back. Lift your legs to a 60-degree angle, then bend and extend your knees for a duration of 30 to 60 seconds. A foot with an inadequate blood supply may hurt or turn pale.
What is the best exercise for peripheral artery disease?
Walking is one of the finest workouts for PAD. After you overcome the early difficulties, this low-impact exercise raises your heart rate and, in the long run, can help with mobility improvement. When you first start, you can feel a little uncomfortable, but that will pass as you walk.

Conclusion
reason for peripheral artery disease
To sum up, peripheral artery disease (PAD) symptoms are important markers of underlying vascular health problems. The appearance of symptoms during physical exercise, such as leg pain, cramping, numbness, and weakness, emphasises the reduced blood supply to the limbs. In addition, non-healing lesions, temperature or colour changes in the skin, and a decreased pulse in the limbs are other indicators that PAD is progressing. Early detection and diagnosis of these symptoms are essential for putting treatments into place on time and reducing the chance of serious side effects like tissue damage and limb loss. Ultimately, improving quality of life and lowering morbidity related to peripheral artery disease require early detection and aggressive management techniques.
So, this is how the topic “peripheral artery disease symptoms” has been addressed.
For more information related to these topics,
You may also visit our Instagram page by
Thank you!